NSCLC cancer may benefit more from surgery, but SCLC results remain the same.
Lung cancer is one of the most common types of cancer in the world, and it is responsible for a significant number of cancer-related deaths each year. The two main treatment options for lung cancer are surgery and radiation therapy, but which of these treatments is more effective in improving survival rates for patients with lung cancer? Recent studies have shed light on this question, suggesting that surgery may be more effective than radiation therapy for certain types of lung cancer. In a study published in the New England Journal of Medicine, researchers compared the effectiveness of surgery and radiation therapy in treating patients with early-stage non-small cell lung cancer (NSCLC). The study included 499 patients with NSCLC who were randomly assigned to receive either surgery or radiation therapy as their initial treatment. The results of the study showed that patients who underwent surgery had a higher overall survival rate than those who received radiation therapy.
The study found that the five-year overall survival rate was 92.5% for patients who underwent surgery, compared to 78.7% for patients who received radiation therapy. The study also found that the rate of recurrence was lower among patients who underwent surgery, with a recurrence rate of 18.6%, compared to 36.3% for patients who received radiation therapy.
The study’s findings are significant because they suggest that surgery may be a more effective treatment option for patients with early-stage NSCLC. However, it is important to note that surgery is not always an option for patients with lung cancer, particularly those who have advanced-stage disease or other health conditions that make surgery too risky.
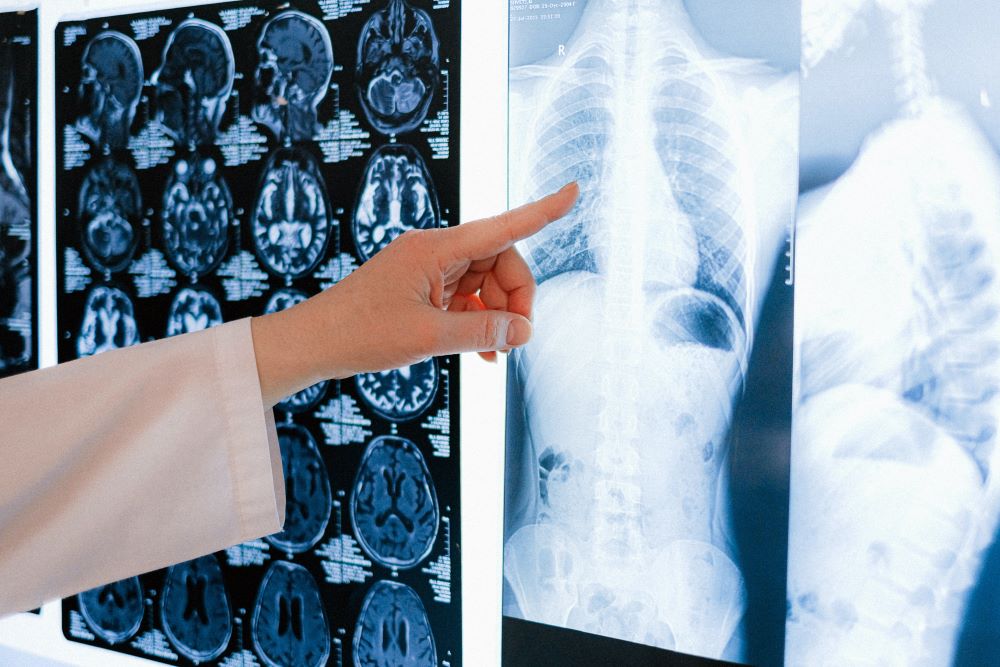
Another study, published in the Journal of the National Cancer Institute, compared the effectiveness of surgery and radiation therapy in treating patients with small cell lung cancer (SCLC). The study included 820 patients with SCLC who were treated with either surgery or radiation therapy as their primary treatment. The results of the study showed that there was no significant difference in overall survival rates between the two treatment options.
The study found that the five-year overall survival rate was 23.2% for patients who underwent surgery, compared to 21.5% for patients who received radiation therapy. The study also found that there was no significant difference in the rate of recurrence or progression-free survival between the two treatment options.
The findings of this study suggest that both surgery and radiation therapy may be equally effective treatment options for patients with SCLC. However, it is important to note that SCLC is often more aggressive than NSCLC and is typically treated with a combination of chemotherapy and radiation therapy.
It is also worth noting that surgery and radiation therapy are not the only treatment options for lung cancer. Other treatment options for lung cancer may include chemotherapy, immunotherapy, targeted therapy, and palliative care.
Overall, the effectiveness of surgery and radiation therapy in treating lung cancer depends on the type and stage of the cancer, as well as the individual patient’s health and other factors. For patients with early-stage NSCLC, surgery may be a more effective treatment option than radiation therapy, while for patients with SCLC, both surgery and radiation therapy may be equally effective. Ultimately, the decision of which treatment option to pursue should be made on a case-by-case basis in consultation with a patient’s healthcare team.
Sources:
Surgery boosts survival rates better than radiation for patients with lung cancer


Join the conversation!