Researchers reveal promising opioid alternative results.
UT Southwestern researchers have shared that long-used antibiotics, when administered together, can block a type of pain associated with nerve damage. The findings were published online in PNAS and could offer an alternative to addictive opioids. Currently, “over 100 million Americans are affected by chronic pain, and a quarter of these experience pain on a daily basis, a burden that costs an estimated $600 billion in lost wages and medical expenses each year,” they noted.
Study leader Enas S. Kandil, M.D., associate professor of anesthesiology and pain management at UTSW, explained, “Despite the desperate need for safer pain medications, development of a new prescription drug typically takes over a decade and more than $2 billion according to a study by the Tufts Center for the Study of Drug Development.”

Seeking an alternative treatment plan for nerve pain, Kandil, along with colleagues Hesham A. Sadek, M.D., Ph.D., professor of internal medicine, molecular biology, and biophysics; Mark Henkemeyer, Ph.D., professor of neuroscience; Mahmoud S. Ahmed, Ph.D., instructor of internal medicine; and Ping Wang, Ph.D., a postdoctoral researcher, took a look at some of the drugs that have already been approved and were available for use in the market.
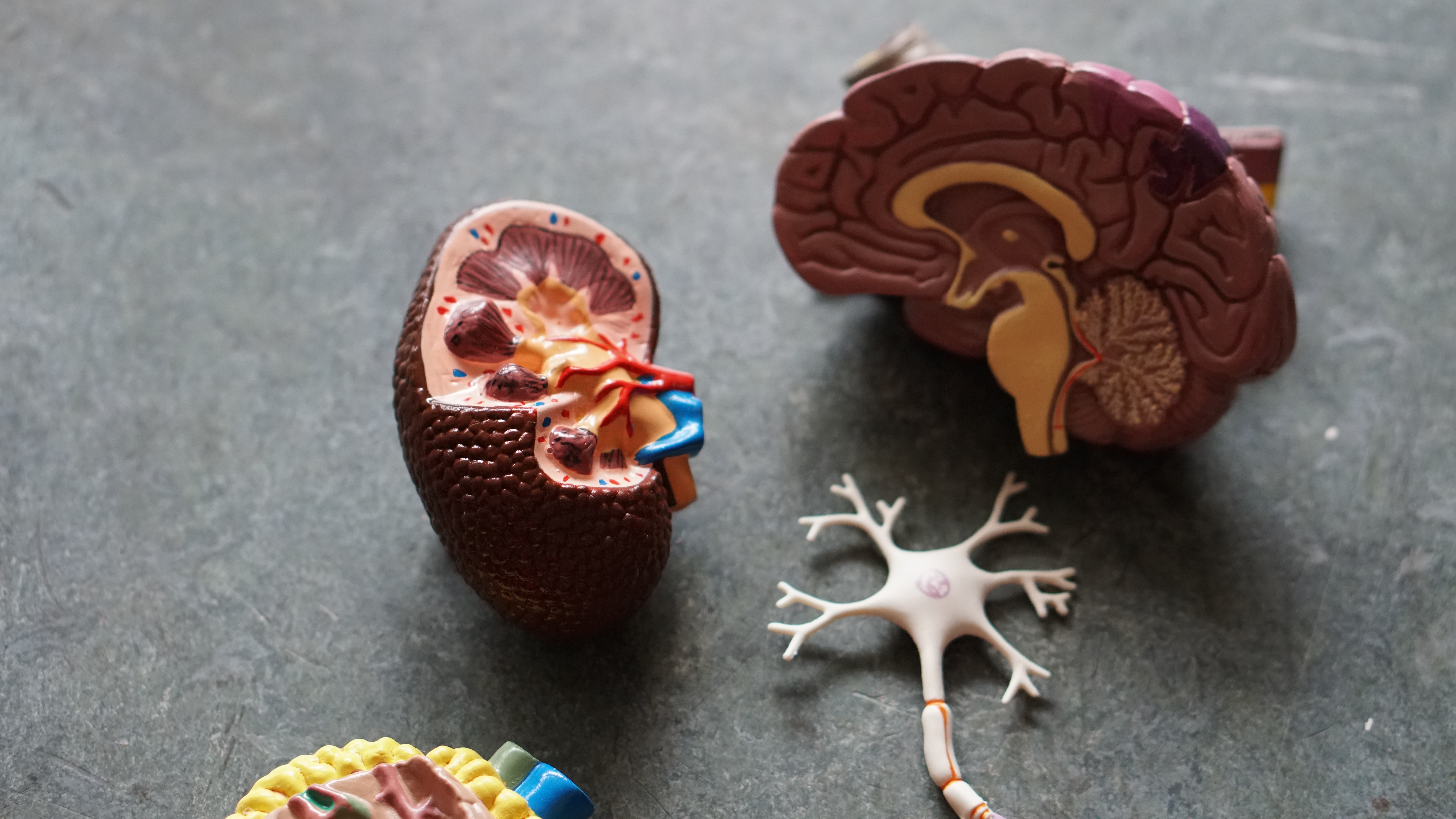
The team focused on EphB1, a protein found on the surface of nerve cells, which has been shown to block neuropathic pain. “Mice genetically altered to remove all EphB1 don’t feel neuropathic pain,” Henkemeyer said. “Even mice with half the usual amount of this protein are resistant to neuropathic pain, suggesting EphB1’s promise as a target for pain-relieving drugs.”
“Exploring this angle further, Ahmed used computer modeling to scan a library of FDA-approved drugs, testing if their molecular structures had the right shape and chemistry to bind to EphB1. Their search turned up three tetracyclines, members of a family of antibiotics used since the 1970s. These drugs – demeclocycline, chlortetracycline, and minocycline – have a long history of safe use and minimal side effects,” Ahmed added.
The researchers published in their report, “Previous studies have demonstrated that the synaptic EphB1 receptor tyrosine kinase is a major mediator of neuropathic pain, suggesting that targeting the activity of this receptor might be a viable therapeutic option. Therefore, we set out to determine if any FDA-approved drugs can act as inhibitors of the EphB1 intracellular catalytic domain…[I]n vivo administration of the three-tetracycline combination inhibited the phosphorylation of EphB1 in the brain, spinal cord, and dorsal root ganglion (DRG) and effectively blocked neuropathic pain in mice. These results indicate that demeclocycline, chlortetracycline, and minocycline can be repurposed for treatment of neuropathic pain and potentially for other indications that would benefit from inhibition of EphB1 receptor kinase activity.”
Kandil explained further how the combination was able to eliminate pain and how this will be beneficial for helping to curtail the opioid crisis, saying, “In three different mouse models of neuropathic pain, injections of these three drugs in combination significantly blunted reactions to painful stimuli such as heat or pressure, with the triplet achieving a greater effect at lower doses than each drug individually…A combination of these drugs might be able to blunt pain in humans too, the next stage for this research. Unless we find alternatives to opioids for chronic pain, we will continue to see a spiral in the opioid epidemic.”
Sources:
Three longtime antibiotics could offer alternative to addictive opioid pain relievers

Join the conversation!